Preeclampsia, also known as “toxemia of pregnancy”, is a serious blood pressure disorder that can occur during pregnancy or shortly after childbirth. It is a leading cause of death worldwide for women, fetuses, and newborns, as it is responsible for over 70,000 maternal deaths and 500,000 fetal deaths every year and affects approximately 5% to 7% of all pregnancies [1]. Preeclampsia is characterized by elevated blood pressure and high protein levels in the urine. The condition may be associated with severe short and long-term effects for both mother and baby [2].
Contents
Diagnosis and symptoms
The first symptoms of preeclampsia usually become apparent mid-pregnancy, after the 24th week of pregnancy, and rarely before the 20th week. Although less common, the mother may develop preeclampsia for the first time in the weeks immediately after birth. Most pregnant women with the condition only experience mild symptoms and feel no discomfort at the beginning, but severe complications may develop without early diagnosis and clinical management. During the first trimester prenatal appointments, a healthcare professional checks the mother for high blood pressure and protein in the urine [1, 2], which are some of the early signs of preeclampsia. These clinical findings in combination with some risk factors, like having an existing medical problem or family history of the condition, help the healthcare professional identify whether the expecting mother has an increased risk of developing preeclampsia.
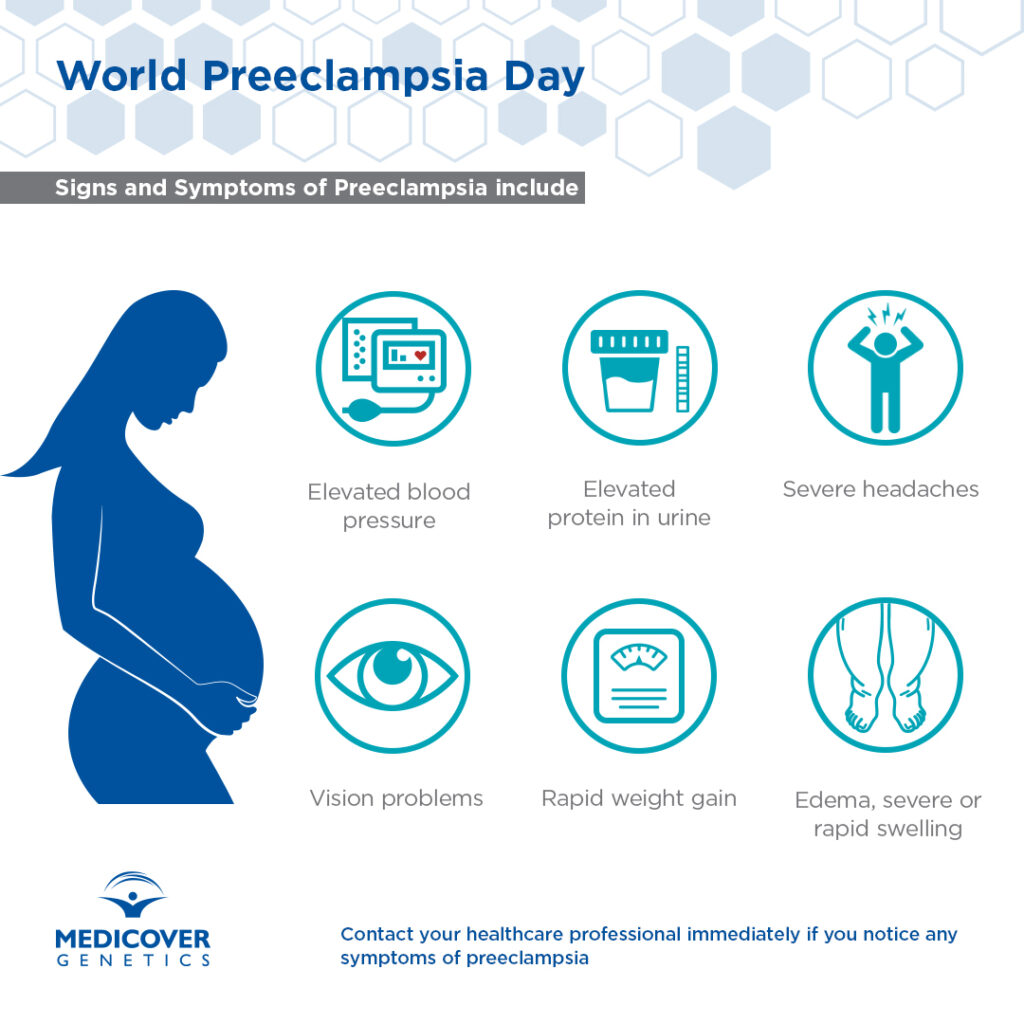
The main sign of preeclampsia in the fetus is slow growth, as the condition prevents the fetus from being adequately nourished and supplied with oxygen due to the poor blood supply through the placenta to the baby [2]. If the condition is not identified from an early stage and progresses, the expecting mother may develop severe headaches or vision problems like sensations of flashing lights, light sensitivity, or blurry vision or spots. Additional symptoms include severe heartburn, nausea or vomiting, rapid and excessive weight gain, pain just below the ribs, sudden or severe swelling of the feet, ankles, face, and hands (edema). Every pregnant woman must be informed about these symptoms and get medical advice immediately if they notice any of them. Without prompt treatment, preeclampsia may lead to rare, yet life-threatening complications for the mother, including organ damage and death. Preeclampsia is also associated with a high risk of the baby being born too small and with low birth weight.
Causes and risk factors
Despite intensive research over the last decades, the exact cause of preeclampsia isn’t fully understood; however, it is thought to be caused by the placenta not developing properly [2]. Many factors can increase the risk of developing preeclampsia, including having a pre-existing medical problem such as diabetes, kidney disease, high blood pressure, or autoimmune conditions like lupus or antiphospholipid syndrome. Also, if a woman had preeclampsia in a previous pregnancy, there is approximately a 16% chance of developing the condition again in later pregnancies. Some factors cumulatively increase a woman’s chances of developing preeclampsia. These include being pregnant for the first time if it has been at least 10 years since the last pregnancy, family history of the condition (mother or sister), whether a woman is over 40, if a woman was obese at the start of her pregnancy with body mass index (BMI) of 35 or more, or if having multiple pregnancies.
Genetics and preeclampsia
It is generally considered that some women are genetically predisposed to preeclampsia and twin studies have estimated the overall heritability to be around 55%. Determining how genetics influences the development of preeclampsia is complicated and must consider the genotype of both the mother and the fetus, which includes genes from both parents.
Preeclampsia is thought to be a complex genetic disorder, where cumulative effects of genetic variants carried by the parents or the fetus affect the tendency to develop the disease. Environmental factors, such as maternal age or weight further influence the effects of genetic variants and disease susceptibility [6].
It has also been reported that a genetic predisposition to hypertension contributes to the risk of preeclampsia. The authors of a recent genome-wide association study of European and Central Asian mothers reported that five variants in the maternal genome previously found to be associated with blood pressure were associated with preeclampsia. They concluded that a number of variants affect the genetic predisposition to preeclampsia by affecting blood pressure regulation [7].
As mentioned above the fetal genome must also be considered, and a genome-wide association study of offspring from preeclamptic pregnancies successfully identified a region of the fetal genome near the FLT1 gene on chromosome 13 that is associated with increased risk for preeclampsia. The researchers identified a single nucleotide polymorphism that conferred preeclampsia risk regardless of whether it came to the fetus from the mother or father, which provided scientists with new evidence for the polygenic nature of preeclampsia [8, 9].
Latest studies about diagnosis of preeclampsia
Apart from the first-trimester routine checks which are performed between the 11th and 14th week of pregnancy to estimate the risk for preeclampsia, newer studies show that determining the ratio of two placental proteins (sFlt-1/PlGF) with a blood test between the 20th and 34th week can predict the onset of preeclampsia about four weeks in advance [4, 5]. Based on this information, if preeclampsia is suspected, the healthcare professional can schedule the frequency of prenatal appointments accordingly, for more careful monitoring and early diagnosis. Monitoring may include keeping track of the fetus’s movements by doing a daily kick count, measuring the blood pressure at home, and scheduling weekly prenatal check visits to check the fetus’s growth.
Treatment
If preeclampsia is confirmed, frequent monitoring by a healthcare professional is essential. Preeclampsia can only be cured by delivering the baby and the placenta [2]. Treatment aims to prolong pregnancy and avoid premature birth, as long as it is safe for both the mother and the baby. If needed, staying in the hospital until the baby can be delivered will be recommended for careful monitoring and early action. Although preeclampsia usually improves soon after the baby is born, complications can sometimes develop a few days later. If preeclampsia is severe, it may cause long-term health consequences for the mother and her baby. On average, 1 in 3 women with severe preeclampsia develops chronic high blood pressure years after their pregnancy and frequently suffers from cardiovascular diseases (CVD) and blood clotting disorders [1, 2]. As babies may be born prematurely, they may experience breathing difficulties caused by undeveloped lungs [2]. To prevent this from happening, healthcare professionals may give injections of corticosteroid medicine to pregnant women to speed up the development of the fetus’s lungs, brain, and kidneys and surfactant production. In newborns with underdeveloped lungs and breathing difficulties, treatment ― surfactant replacement therapy, breathing support from a ventilator, or other supportive cures ― should begin immediately. Most babies who show signs of a breathing disorder are quickly moved to a neonatal intensive care unit (NICU) to receive constant treatment.
Prevention
Currently, there is no single diagnostic test that can accurately predict if a woman will develop preeclampsia during pregnancy or right after childbirth. Therefore, raising awareness to prevent preeclampsia is the most powerful tool for the successful, early recognition and clinical management of the condition [3]. This involves identifying risk factors for preeclampsia, informing women of the signs and symptoms, and stressing the importance of contacting a healthcare professional as soon as possible. It is crucial for pregnant women to attend all their prenatal appointments, monitor their blood pressure at every prenatal check or at home, and be aware of specific warning signals such as headaches, impaired vision or rapid weight gain, fluid retention, or restlessness. Maintaining a healthy eating lifestyle, staying physically active, and avoiding stress are vitally important for the prevention and good management of preeclampsia.
Conclusion
Preeclampsia, characterized by elevated blood pressure and high protein levels in the urine usually becomes apparent mid-pregnancy. It can have long-term health consequences for the mother and her baby and is a leading cause of death for women, fetuses, and newborns worldwide. There are a number of known risk factors for preeclampsia, such as increased maternal age or weight, and research continues to investigate causal genetic variations and research the complex, polygenic nature of the disease.
Please note: The content is intended only for educational purposes and should not be perceived as medical advice.
References
[1] Rana S et al. Preeclampsia: Pathophysiology, Challenges, and Perspectives. Circ Res 2019 Mar 29;124(7):1094-1112. doi: 10.1161/CIRCRESAHA.118.313276. Erratum in: Circ Res. 2020 Jan 3;126(1):e8. PMID: 30920918. https://www.ahajournals.org/doi/10.1161/CIRCRESAHA.118.313276
[2] Bokslag A et al. Preeclampsia; short and long-term consequences for mother and neonate. Early Hum Dev 2016 Nov;102:47-50. doi: 10.1016/j.earlhumdev.2016.09.007. Epub 2016 Sep 20. PMID: 27659865. https://www.sciencedirect.com/science/article/abs/pii/S0378378216304030
[3] Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists’ Task Force on Hypertension in Pregnancy. Obstet Gynecol 2013 Nov;122(5):1122-1131. doi: 10.1097/01.AOG.0000437382.03963.88. PMID: 24150027. https://journals.lww.com/greenjournal/Fulltext/2013/11000/Hypertension_in_Pregnancy__Executive_Summary.36.aspx
[4] European Foundation for the Care of Newborn Infants (EFCNI). act early! screen early! – raising awareness for pre-eclampsia 2022. Retrieved 22 May 2022 from https://www.efcni.org/activities/campaigns/world-preeclampsia-day/
[5] Chau K et al. Placental growth factor and pre-eclampsia. J Hum Hypertens 2017 Dec;31(12):782-786. doi: 10.1038/jhh.2017.61. Epub 2017 Aug 24. PMID: 29115294; PMCID: PMC5680413. https://www.nature.com/articles/jhh201761
[6] Williams PJ et al. The genetics of pre-eclampsia and other hypertensive disorders of pregnancy. Best Pract Res Clin Obstet Gynaecol 2011 Aug;25(4):405-17. doi: 10.1016/j.bpobgyn.2011.02.007. Epub 2011 Mar 22. PMID: 21429808; PMCID: PMC3145161. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC3145161/
[7] Steinthorsdottir, V et al. Genetic predisposition to hypertension is associated with preeclampsia in European and Central Asian women. Nat Commun 2020 11:5976. https://doi.org/10.1038/s41467-020-19733-6
[8] McGinnis, R et al. Variants in the fetal genome near FLT1 are associated with risk of preeclampsia. Nat Genet 2017 49:1255–1260. https://doi.org/10.1038/ng.3895 https://www.nature.com/articles/ng.3895
[9] Gray KJ et al. Genetic predisposition to preeclampsia is conferred by fetal DNA variants near FLT1, a gene involved in the regulation of angiogenesis. Am J Obstet Gynecol 2018 218(2):211-218. doi: 10.1016/j.ajog.2017.11.562. Epub 2017 Nov 11. PMID: 29138037; PMCID: PMC5807126. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC5807126/pdf/nihms930794.pdf
Additional references
European Foundation for the Care of Newborn Infants (EFCNI). act early! screen early! – raising awareness for pre-eclampsia 2022. Retrieved 22 May 2022 from https://www.efcni.org/activities/campaigns/world-preeclampsia-day/
NHS. Pre-eclampsia. Retrieved 22 May 2022 from https://www.nhs.uk/conditions/pre-eclampsia/
ACOG. Preeclampsia and Pregnancy. Retrieved 22 May 2022 from https://www.acog.org/womens-health/infographics/preeclampsia-and-pregnancy
ACOG. Preeclampsia and High Blood Pressure During Pregnancy. Retrieved 22 May 2022 from https://www.acog.org/womens-health/faqs/preeclampsia-and-high-blood-pressure-during-pregnancy
NHLBI. Respiratory Distress Syndrome. Retrieved 22 May 2022 from https://www.nhlbi.nih.gov/health-topics/respiratory-distress-syndrome
NIHR. Placental growth factor testing can speed up diagnosis of pre-eclampsia. Retrieved 22 May 2022 from https://evidence.nihr.ac.uk/alert/placental-growth-factor-testing-can-speed-up-diagnosis-of-pre-eclampsia/