Arrythmogenic diseases include primary arrythmia syndromes, which are ion channel diseases of the heart muscle, and cardiomyopathies with a risk of arrythmia. The three most common ion channel diseases are long QT syndrome (LQTS), Brugada syndrome (BrS) and catecholaminergic polymorphic ventricular tachycardia (CPVT). The most important cardiomyopathies are hypertrophic cardiomyopathy (HCM), dilated cardiomyopathy (DCM) and arrythmogenic right ventricular cardiomyopathy (ARVC). Other types of cardiomyopathy are
restrictive cardiomyopathy (RCM) and non-compaction cardiomyopathy (NCCM).
Most forms of these diseases follow an autosomal dominant inheritance pattern with incomplete penetrance and variable expression. The most important pathogenic genes have been known for several years. In most cases, genetic diagnosis is considered useful (see Ackerman et al, Europace 13:1077, 2011). It often serves to confirm the diagnosis, but can also have prognostic or therapeutic significance. Following identification of the pathogenic mutation in the index case, the targeted analysis of blood relatives is paramount for ion channel diseases. Due to the therapeutic consequences, predictive diagnostics is also recommended without restriction for minors. In cardiomyopathies on the other hand, the indication for predictive diagnostics should be carefully considered as part of genetic counselling, especially in the case of minors. Checking for genetic segregation within the family can be helpful for the interpretation of some variants.
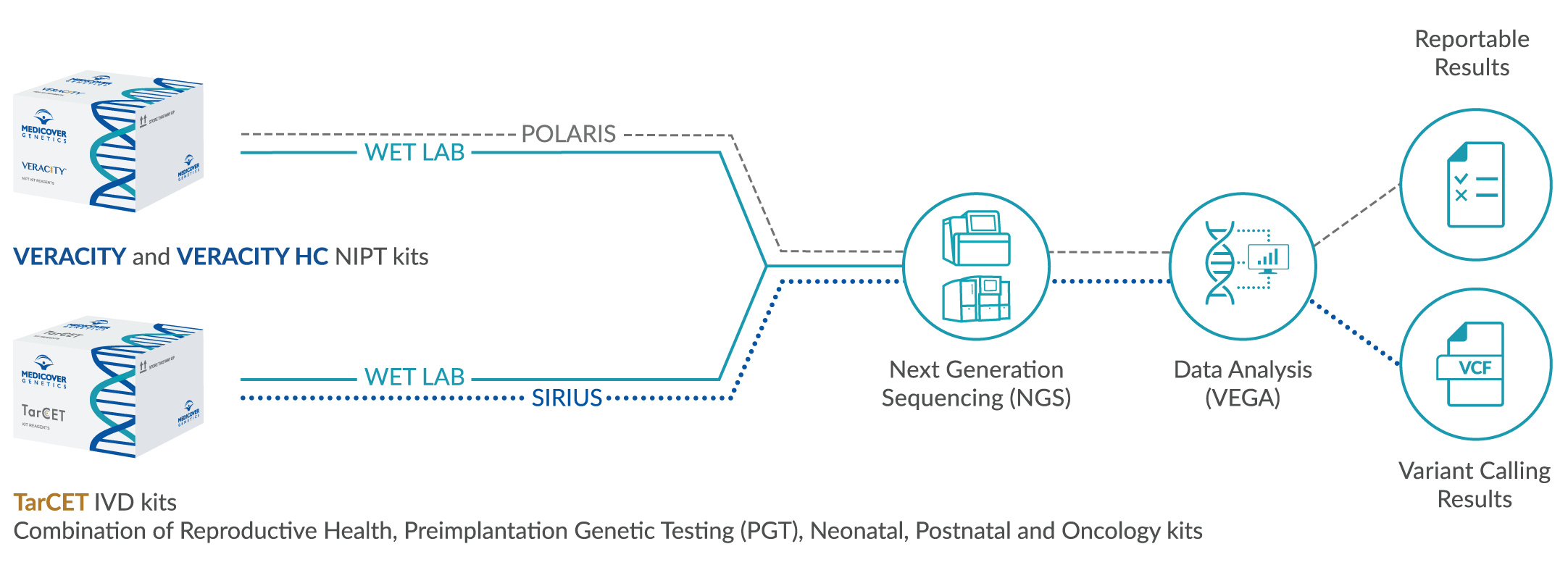
The molecular genetic diagnosis of all arrythmogenic diseases available here is based on DNA sequencing of the known pathogenic genes (gene panel diagnostics). The analysis or evaluation of the results is indication-specific and is performed in stages. In recent years, the number of genes that are causally related to arrythmogenic diseases has increased dramatically. Nevertheless, in ion channel diseases (LQTS, BrS, CPVT) and ARVD, 90-95% of variants are found in a few major genes even when all known genes are analyzed. In order to achieve the highest possible diagnostic sensitivity, it may therefore make more sense, as in LQTS, to examine the main genes KCNQ1, KCNH2 and SCN5A for large deletions than to analyze all known genes. In addition, the analysis of rarely affected genes often leads to unclear results or additional findings. Consequently, current diagnostic recommendations are often limited to the main genes. In contrast to ion channel diseases, the causes of HCM and DCM are much more heterogeneous. In this case, gene panel diagnostics using NGS is a good option. This technology enables the parallel analysis of more than 50 genes currently considered cardiologically relevant in one approach. This includes titin (TTN), the largest human gene, which has a causal connection in about 25% of DCM cases. However, the interpretation of the NGS results is still a major challenge. For example, a validation of TTN variants by segregation analyses is currently necessary. Therefore, the analysis of this gene should possibly be limited to larger families with several affected persons. The use of NGS is also advantageous in selected cases of ion channel diseases when the differential diagnosis is difficult and there are several suspected diagnoses.
Genetic analysis for cardiomyopathies should be considered in the following situations:
- Family history: A family history of cardiomyopathic disease is common.
- Symptoms/conspicuous imaging: The patient shows clinical symptoms that can be attributed to a cardiomyopathy or the echocardiography/cardio-MRI revealed indications of the presence of a cardiomyopathy.
- Prevention: Genetic analysis may be useful for early diagnosis and prevention of complications in relatives of patients with genetically confirmed cardiomyopathies.
Genetic analysis can help to confirm the diagnosis, identify patients at risk, and develop targeted therapeutic measures or preventive strategies.
References
Medeiros-Domingo et al. 2016, Europace pii: euw098 / Schulze-Bahr et al. 2015, Kardiologe DOI 10.1007/s12181-014-0636-2 / Mogensen et al. 2015, Eur Heart J 36:1367 / Abriel et al. 2013, Gene 517:1 / Beckmann et al. 2013, pädiat prax 80:31 / Campuzano et al. 2013, J Med Genet 50:280 / Sikkema-Raddatz et al. 2013, Human Mutat online April / Kaufman et al. 2012, JACC 60:1419 / Herman et al. 2012, N Engl J Med 366:619 / Ackerman et al. 2011, Europace 13:1077 / Tester et al. 2010, Am J Cardiol 106:1124