Prostate carcinoma (PCa) is the most common non-cutaneous cancer in men worldwide, with about 1.6 million cases and 366,000 deaths annually. Approximately 80% to 90% of all PCa arise in the peripheral zone of the prostate, about 10% in the transition zone, and few in the other three areas of the prostate (central, anterior, around the urethra). Three stages of development have been identified: (a) intraepithelial neoplasia, which can be considered precancerous and is characterized by hyperplasia of luminal cells and progressive loss of basal cells; (b) adenocarcinoma androgen-dependent (divided into two stages: latent and clinical), characterized by complete loss of basal cells and luminal phenotype: At this stage, the tumor is androgen-dependent and its growth can be controlled by androgen deprivation; and (c) adenocarcinoma androgen-independent (or castration-resistant).
GENOMIC ALTERATIONS AND POSSIBLE THERAPIES
With early diagnosis and treatment, patients have a good prognosis. Treatment of PCa depends on the grade, stage, and age and ranges from active surveillance to a mixture of surgery, chemotherapy, radiation, and/or androgen deprivation therapy (ADT). ADT is often used in combination with surgery or radiation, and often in combination with chemotherapy for metastatic disease. ADT may include two approaches: surgical castration (orchiectomy) or chemical castration with drugs that target the AR pathway.
Although most patients initially respond well to this therapy, nearly all cases recur and progress to primary castration-resistant prostate cancer (CRPC) or metastatic CRPC (mCRPC). For example, if this resistance is based on an alteration in AR, in NCOR1/2, or in FOXA1, therapy with AR inhibitors (e.g., enzalutamide) or CYP17A1 inhibitors (e.g., abiraterone) may prolong overall survival.
Approximately 25% of mCRPC patients demonstrate homologous DNA repair (HRR) deficiency and may benefit from therapy with poly (ADP-ribose) polymerase (PARP) inhibitors (PARPi).
The greatest benefit of PARPi therapy appears to be shown by mCRPC patients with a change in BRCA1 or BRCA2, whereas patients with variants in ATM and CDK12 show limited response. However, patients with CDK12 inactivation may benefit from therapy with immune checkpoint inhibitors alone or in combination with PARPi due to an increased neoantigen load. Variants in the other HRR genes have a relatively low prevalence in mCRPC. Potential combination therapy of PARPi and second-generation antiandrogens could increase response, if appropriate.
Two PARPi for the treatment of PCa have been approved by the FDA: Olaparib for mCRPC patients who have previously received a second-generation hormonal agent and have a variant in an HRR gene (BRCA1, BRCA2, ATM, BARD1, BRIP1, CDK12, CHEK1, CHEK2, FANCL, PALB2, RAD51B, RAD51C, RAD51D, RAD54L); Rucaparib for mCRPC patients who have previously received a second-generation hormonal agent or taxane chemotherapy and have a variant in BRCA or BRCA2.
A family history of PCa increases the risk for PCa. In addition, PCa has been associated with hereditary breast and ovarian cancer (HBOC) syndrome (due to germline variants in homologous DNA repair genes) and Lynch syndrome (due to germline variants in DNA mismatch repair genes). Indeed, approximately 11% of patients with PCa and at least one additional primary tumor in the family carry germline variants that are associated with an increased risk of cancer. Therefore, we recommend a thorough review of personal and family history for all patients with PCa and patient education.
TEST RECOMMENDATIONS
Guidelines recommend tumor testing for variants in HRR genes (BRCA1, BRCA2, ATM, CHEK2, PALB2, FANCA, RAD51D, CDK12) and determination of microsatellite instability (MSI) or mismatch repair status (MLH1, MSH2, MSH2, PMS2) in all men with regional or metastatic high-risk prostate cancer. In cases of high MSI (MSI-H), therapy with immune checkpoint inhibitors may be considered, as pembrolizumab has been approved by the FDA for the treatment of non-resectable or metastatic solid tumors with dMMR or MSI-H. Targeted germline testing can be linked to identify patients with family members who may be at increased risk for cancer.
A TMPRSS2-ERG translocation is found in approximately 15% of prostate intraepithelial neoplasia (PIN) and in approximately 50% of PCa patients. Other translocations of the ETS family have been described, TMPRSS2-ERG-positive tumors exhibit some special features related to androgen metabolism. They have increased androgen-regulated gene expression and altered intratumoral androgen metabolism, as demonstrated by decreased testosterone concentrations and increased dihydrotestosterone (DHT)/testosterone ratios. Therefore, patients with TMPRSS2-ERG-positive PCa may benefit from novel inhibitors targeting alternative DHT biosynthesis. In the future, PARPi may also play a role in PCa patients with TMPRSS2-ERG translocation because PARP1 can interact with ERG. The resulting ERG overexpression could be inhibited by PARPi and the growth of ERG-positive tumor cells slowed.
Approximately 15% of PCa show variants in SPOP with favorable prognosis and improved progression-free survival, especially in patients with high PSA levels before treatment. There is also evidence that SPOP-mutated PCa fail to degrade PD-L1 due to a lack of binding to PD-L1, which may support the use of immunotherapy with immune checkpoint inhibitors in these tumors.
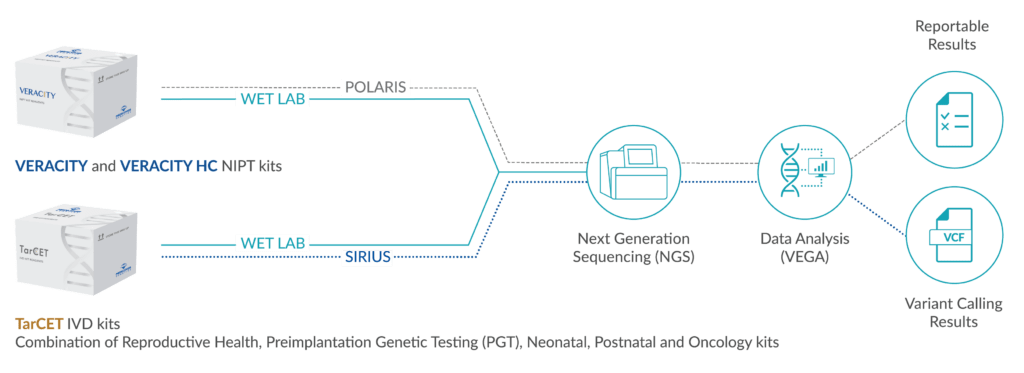
GENE PANEL
27 genes: AKT1, AR, ATM, ATR, BARD1, BRCA1, BRCA2, BRIP1, CDK12, CHEK1, CHEK2, FANCA, FANCL, FOXA1, IDH1, MYC, NCOR1, PALB2, PIK3CA, PTEN, RAD51B, RAD51C, RAD51D, RB1, SMAD4, SPOP, TP53
FUSION GENE PANEL
ESRP1-RAF1, RAF1-ESRP1, SLC45A3-BRAF, SND1-BRAF, TMPRSS2-ERG, UBE2L3-KRAS
TARGETED PANEL
ATM, BRCA1, BRCA2, CDK12, CHEK2, FANCA, PALB2, PTEN, RAD51, MSI